
Physical Therapy with an External Fixator
Proven, Innovative Treatment for Your Child With a Limb Length Discrepancy
When an external fixator (EXFIX) is used to help treat your child's limb length discrepancy, physical therapy is essential in ensuring a successful outcome for your child. Physical therapy combined with an EXFIX can help create the best quality of life for your child.
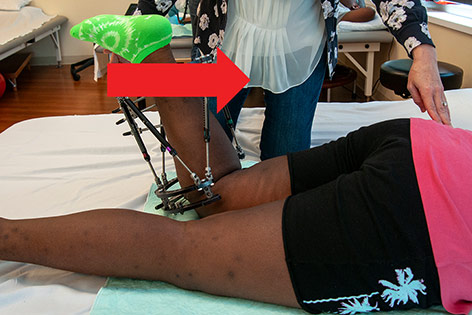
During limb lengthening surgery, the process begins with an osteotomy, during which a skilled Shriners Children's orthopedic surgeon cuts the bone to be lengthened. The surgeon then stabilizes the limb using one of several different external fixation devices, called frames. The device has small rods, called pins, that go through the skin and into the bone.
This treatment is most commonly used on legs, but in some circumstances it can be done on arms as well.
Children with limb length inequalities, along with their families and caregivers, can look forward to a family-centered, multidisciplinary approach to their care at Shriners Children’s. Each treatment plan is individualized to the child’s and family’s specific goals and needs.
Our patients and their families are supported by our own Shriners “family,” our team of skilled, caring, and dedicated surgeons, nurses, orthotists and physical, occupational, and child-life therapists, throughout the continuum of care, and conveniently, all under the same roof.
Custom Treatment Plan Designed Specifically for Your Child
Shriners Children’s understands there is no “one size fits all" solution when it comes to specialized pediatric care.
Your child’s surgeon will work closely with you and the care team to create the best treatment plan to help your child reach his or her goals, and to meet your needs as a family. If a surgical lengthening is recommended, your surgeon will advise whether a lengthening with an external fixator, or with an Ellipse self-lengthening nail, would be the safest and most effective option for your child.
During surgery to lengthen a bone with an external fixator, the surgeon places an external fixator composed of metal rings and adjustable bars, called struts, to allow the gradual lengthening of the limb at the site where the bone has been cut, called an osteotomy or corticotomy. With an external fixator, the rings remain outside of the leg, and the caregiver assists with the lengthening process by turning the struts according to a specific schedule each day.
During surgery to lengthen a bone with a self-lengthening nail, the surgeon places the self-lengthening nail into the bone, and secures it with screws at each end of the nail. With an Ellipse nail, the nail and screws remain completely inside the leg, and the parent or guardian assists with the lengthening process by using an external magnetic device according to a specific schedule each day.
Personalized Physical and Occupational Therapy
An individually designed physical therapy (PT) or occupational therapy (OT) treatment program is a critical component of any successful limb lengthening. You will most likely meet your physical therapist prior to surgery and may be given an exercise program at that time to prepare your child for the lengthening procedure. Each child’s course of therapy will include specific exercises to help stretch muscles and joints and to maximize strength as the limb is lengthened, along with functional activities to improve ease of movement and promote independent mobility and activities of daily living.
Outpatient PT or OT treatments and daily home exercise programs are prescribed while the limb is being lengthened, and continue through a subsequent period of bone healing and rehabilitation, which may continue for a total of six to 12 months on average. Some children will also benefit from a PT or OT exercise program to improve strength and mobility even before surgery, and will be provided with the necessary instruction and recommendations during a preoperative outpatient clinic appointment.
Family Participation in After-Care
Consistent, daily parent or guardian participation in each child’s after-surgery care is crucial to achieving a successful outcome. Parents or guardians participate in the following ways:
- Carefully adhering to the daily lengthening schedule for an external fixator or Ellipse self-lengthening nail
- Assisting your child with a twice daily home physical or occupational therapy exercise program to improve strength and range of motion in the limb being lengthened
- Ensuring your child’s adherence to activity guidelines or restrictions to either promote bone growth or to protect a bone as instructed
- Attending all postoperative clinic appointments with your surgeon, as scheduled
- Attending all postoperative physical or occupational therapy appointments, as scheduled
Shriners Children’s Is Here for You
Children with a more significant limb length discrepancy may require more than one lengthening procedure in order to equalize the limb lengths as much as possible. Whatever your child’s treatment plan, our Shriners Children’s specialized care team, our Shriners family, is here to guide and support you through every step of your journey.
Specific treatments and services may vary by location. Please contact a specific location for more information.
External Fixator Physical Therapy Instructions
General Guidelines

Activity:
- Standing and walking on surgical leg is encouraged! Crutches/walker are for comfort and balance only and may be weaned as able.
- Home exercise program twice daily.
- May use ankle weights and resistance bands under PT guidance.
- May pedal stationary bike, walk on treadmill, use elliptical as tolerated.
- It is safe and generally well-tolerated to lift from the external fixator rings when assisting patient in moving leg.

Positioning/Bracewear:
- Wear ankle brace or dorsiflexion strap as instructed.
- Lie flat on stomach at least once daily for 30 minutes.
- No compression garments or devices. May elevate and ice as needed for swelling.
Strengthening
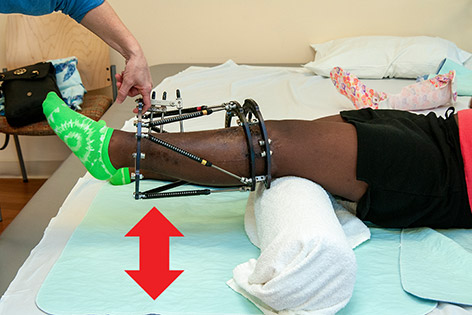
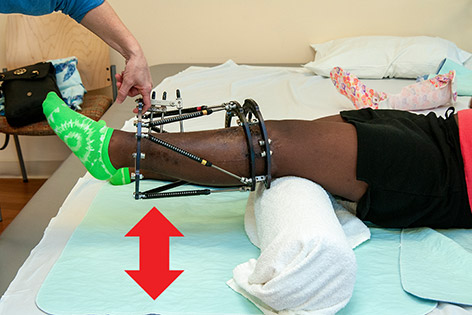
Ankle pumps: With leg resting on bed and knee straight, slowly pump ankle up and down as far as possible.

Quad sets: Tighten thigh muscle and straighten knee as much as possible. Hold 5 seconds.
Glute sets: Tighten buttocks, hold 5 seconds.

Hip abduction: Slide leg slowly out to side, keeping knee straight and pointed towards ceiling.

Hip rotation: Gently roll leg inward and outward, keeping knee straight.

Heel slides: Slowly bend your knee by sliding your foot as close to your buttocks as able.
Short arc quads: Place a firmly rolled blanket under knee, with foot resting on bed. Straighten knee and hold 5 seconds.

Straight leg raise: Lie on your back with opposite knee bent. Slowly raise leg, keeping knee straight. Hold 2 seconds.
Stretching
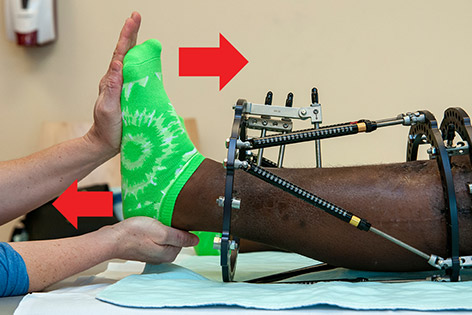
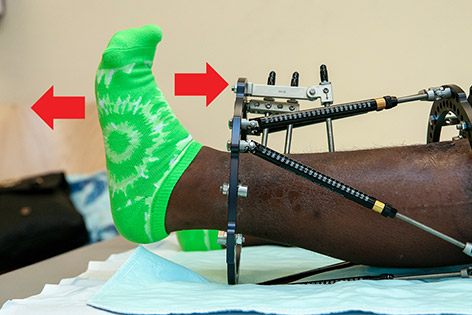
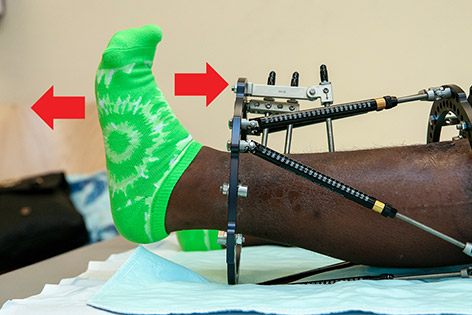
Heelcord stretch: Pull heelbone AWAY from patient while pushing ball of foot TOWARDS patient. Hold 20 seconds.

Knee extension stretch: Gently push down on top of thigh (just above the knee) while lifting calf upward, to straighten knee. Hold 20 seconds.

Hip extension stretch: Lying on side. Stabilize pelvis with one hand firmly on buttocks while slowly moving thigh backwards, to straighten hip. Hold 20 seconds.

Hip abduction stretch: Take leg out to side until a stretch is felt on inner thigh. Keep knee straight. Stabilize hip on opposite side. Hold 20 seconds.
General Guidelines

Activity:
- Standing and walking on surgical leg is encouraged! Crutches/walker are for comfort and balance only and may be weaned as able.
- Home exercise program twice daily.
- May use ankle weights and resistance bands under PT guidance.
- May pedal stationary bike, walk on treadmill, use elliptical as tolerated.

Positioning/Bracewear:
- Wear ankle brace or dorsiflexion strap as instructed.
- Lie flat on stomach at least once daily for 30 minutes.
- No compression garments or devices. May elevate and ice as needed for swelling.
Strengthening
Ankle pumps: With leg resting on bed and knee straight, slowly pump ankle up and down as far as possible.

Quad sets: Tighten thigh muscle and straighten knee as much as possible. Hold 5 seconds.
Glute sets: Tighten buttocks, hold 5 seconds.
Short arc quads: Place a firmly rolled blanket under knee, with foot resting on bed. Straighten knee and hold 5 seconds.

Heel slides: Slowly bend your knee by sliding your foot as close to your buttocks as able.

Long arc quads: Sit with knees bent. Slowly straighten knee. Hold 5 seconds.

Straight leg raise: Lie on your back with opposite knee bent. Slowly raise leg, keeping knee straight. Hold 2 seconds.

Straight leg raise, sidelying: Bend bottom leg. Keep top leg in line with shoulder. Raise leg slowly, keeping knee straight. Hold 2 seconds.

Straight leg raise, prone: Tighten buttocks and raise leg, keeping knee straight. Hold 2 seconds. Optional: Place pillow under hips.

Hamstring curls: Slowly bend knee, bringing foot towards buttocks until you feel a stretch on front of thigh. Hold 5 seconds.

Standing hip flexion with knee bent: Stand with hand on a support. Lift leg with knee bent, as if marching.

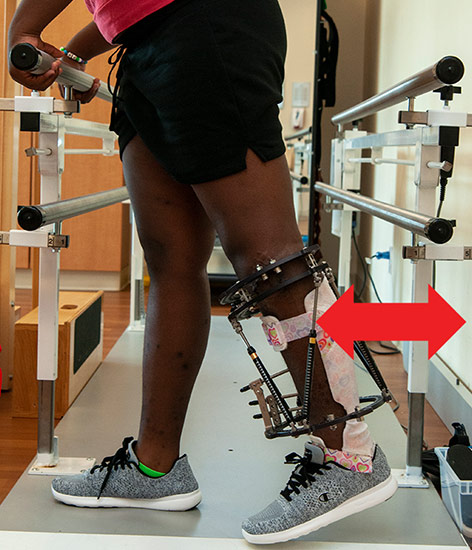
Standing hip abduction: Stand with hand on a support. Tighten outer thigh and lift leg to the side, keeping knee straight and trunk upright.
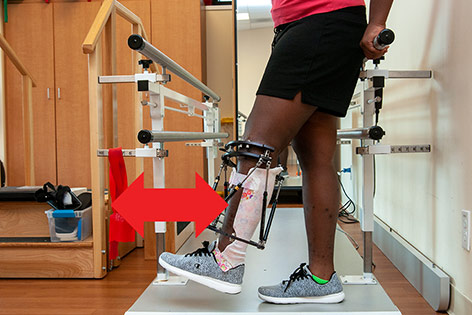
Standing hip extension: Stand with hand on a support. Tighten buttocks and lift leg behind you, keeping knee straight and trunk upright.
Standing hip flexion with knee straight Stand with hand on a support. Lift leg forward, keeping knee straight.

Weight bearing on scale: Practice placing as much weight as tolerated through leg. Use a bathroom scale to measure progress.
Stretching
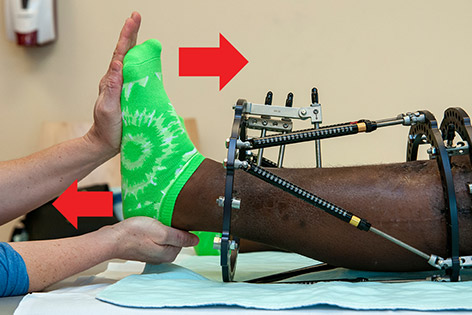
Heelcord stretch: Pull heelbone AWAY from patient while pushing ball of foot TOWARDS patient. Hold 20 seconds.

Knee extension stretch: Gently push down on top of thigh (just above the knee) while lifting calf upward, to straighten knee. Hold 20 seconds.

Hip extension stretch: Lying on side. Stabilize pelvis with one hand firmly on buttocks while slowly moving thigh backwards, to straighten hip. Hold 20 seconds.
Knee flexion stretch: Lying on stomach. Stabilize hip while gently bending knee. Do not allow bottom to rise from bed. Hold 20 seconds.

Hip abduction stretch: Take leg out to side until a stretch is felt on inner thigh. Stabilize hip on opposite side. Keep knee straight and avoid leg rolling outward. Hold 20 seconds.

Hamstring stretch: Begin with hip and knee bent in a chair position. Keeping thigh in place, gently straighten knee until stretch is felt on back of thigh. Hold 20 seconds..
Initially after surgery, kids may feel afraid to move the limb with the external fixator. As the lengthening process begins, their muscles will tighten and weaken somewhat. This is to be expected. The goals of physical therapy are to help keep the child's muscles flexible and strong, and to help them stay as active as possible throughout the rehabilitation process.
Here are some answers to common questions and concerns your child may have:
When does physical therapy start? Physical therapy will begin the day after surgery. Your physical therapist will provide your child with an exercise program that you will help your child perform in their room on weekends. Most kids are able to go home the Monday following surgery.
It it seems too difficult... At first, your child may need help moving their limb in bed. If it involves their leg, this will include standing and taking a few steps with a walker or crutches. Your child likely will require a wheelchair to get to physical therapy. This is perfectly normal and you will work with your child to help them regain their independence. Most kids are up and walking with a walker or crutches by the time they leave the hospital, using a wheelchair only for long distances outside of the home.
How does physical therapy work? While in physical therapy, your child will work on strengthening and stretching exercises. Your physical therapist will provide an exercise program designed specifically for your child and will make recommendations on whether a walker, crutches or cane is best for them. If your child is able, your therapist will teach them how to walk up and down a small flight of stairs in the physical therapy department as well. Things may go slowly the first day or two, but it will get easier.
Will I have to do this at home? Before your child leaves the hospital, your physical therapist will ask you to demonstrate that you're comfortable assisting your child with their home exercise program and supervising them while walking. You'll also be asked to show that you can adjust your child's external fixator. You will be given a written copy of your child's home exercise plan, including your therapist’s contact information in case you have any questions after you leave. It is very important that you encourage your child to continue to perform their exercise plan as instructed and follow all therapy instructions. This is the proven method to give your child the best quality of life.
The care, support and devotion Marie Eva received from Shriners Children's was never interrupted.

Convenient, Skilled Physical Therapy
Services We Provide

Physical Therapy

Occupational Therapy

Motion Analysis

Pediatric Orthotic and Prosthetic Services (POPS)

Care Management

Psychiatry & Psychological Services

